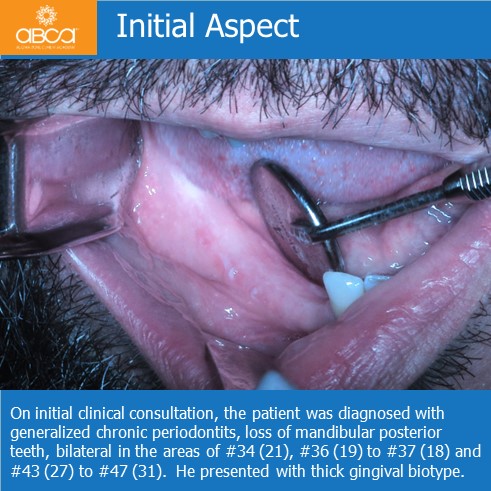
The patient is a nonsmoking, 48-year-old male. He came to the clinic for fixed oral rehabilitation on dental implants. On initial clinical consultation, the patient was diagnosed with generalized chronic periodontits, loss of mandibular posterior teeth, bilateral in the areas of #34 (21), #36 (19) to #37 (18) and #43 (27) to #47 (31).
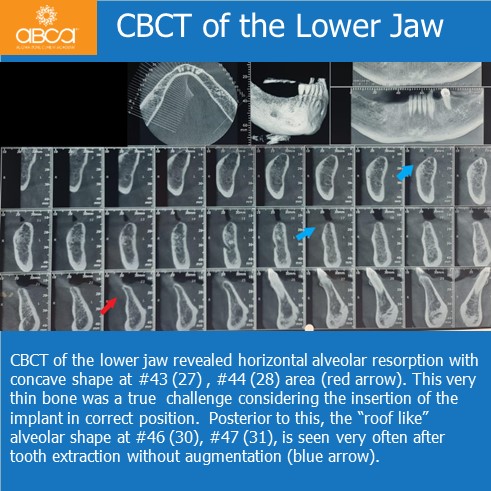
CBCT of the lower jaw revealed horizontal alveolar resorption with concave shape at #43 (27) , #44 (28) area. This very thin bone was a true challenge considering the insertion of the implant in correct position. Posterior to this, the “roof like’’ alveolar shape at #46 (30), #47 (31), is seen very often after tooth extraction without augmentation.
The treatment protocol included as a first step Er- Yag laser assisted treatment of chronic periodontists to stabilize the disease. Only after reduction of the inflammation, 2 weeks after initiating the laser treatment, implants are inserted (Noris Medical Israel) at the location of teeth #43 (27), #44 (28), #46 (30), #47 (31) as well as alveolar regeneration with Augma Bond Apatite® to increase the bone width.
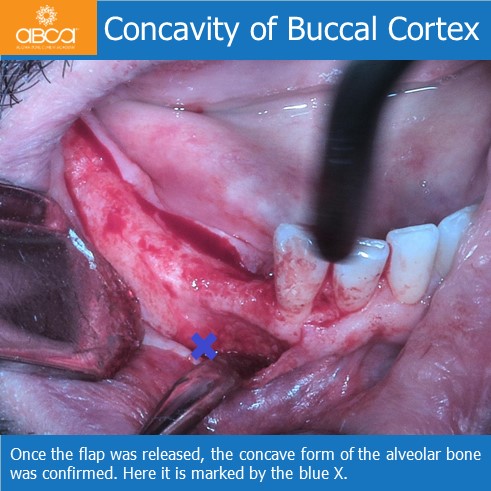
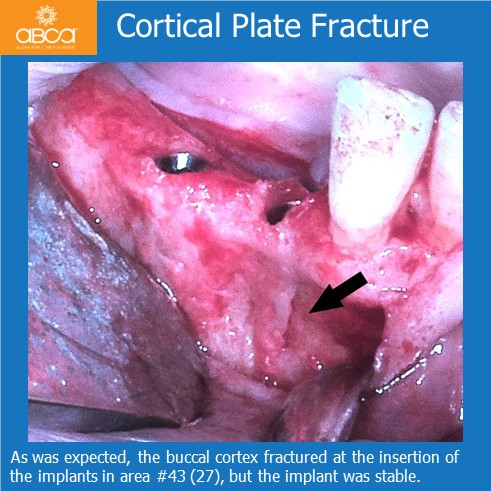
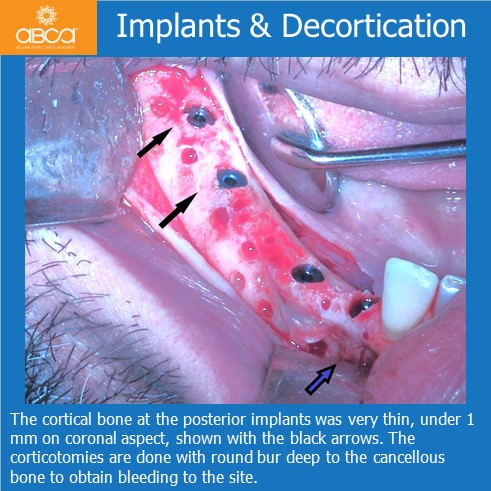
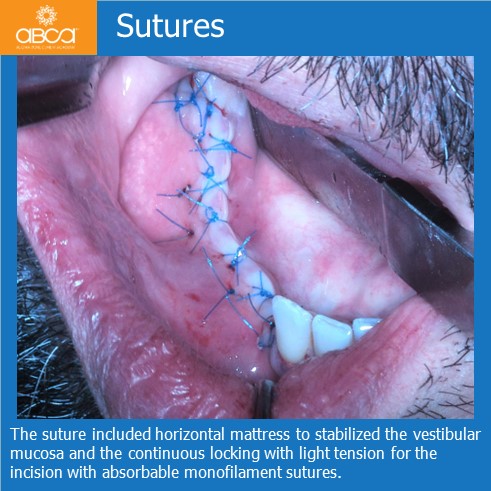
Once the flap was released the concave form of the alveolar bone was confirmed. As was expected, the buccal cortex fractured at the insertion of the implants in area #43 (27), but the implant was stable. The cortical bone at the posterior implants was very thin, under 1 mm on coronal aspect, shown with the black arrows. The corticotomies are done with round bur deep to the cancellous bone to obtain bleeding to the site and Augma Bond Apatite® was added to cover the implants vertical and horizontal. The suture included horizontal mattress to stabilized the vestibular mucosa and the continuous locking with light tension for the incision with absorbable monofilament sutures.
After 5 months the implants were exposed . Buccal cortical wall was regenerated over entire area, and the implants were stable.
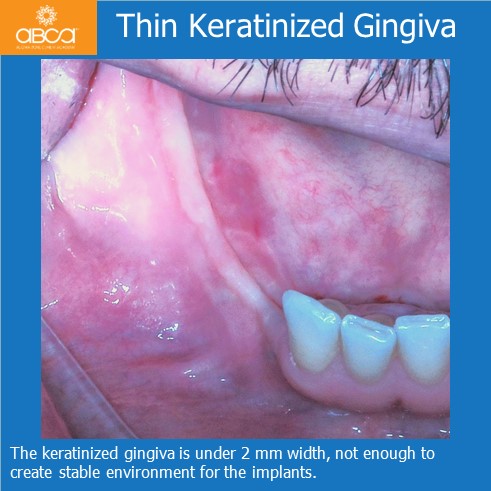
The CBCT revealed the increasing width on posterior area and the correction of the concavity for the anterior implants. There is proof of bone regeneration on the X-ray, and the soft tissue manipulation is with maximum care. The keratinized gingiva is under 2 mm width, not enough to create stable environment for the implants.
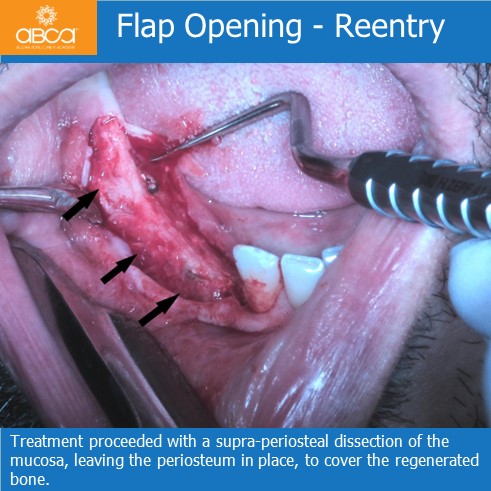
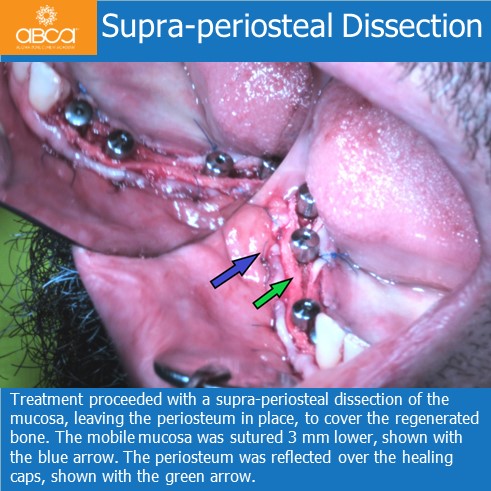
Treatment proceeded with a supra-periosteal dissection of the mucosa, leaving the periosteum in place, to cover the regenerated bone. The mobile mucosa was sutured 3 mm lower, shown with the blue arrow. The periosteum was reflected over the healing caps, shown with the green arrow.
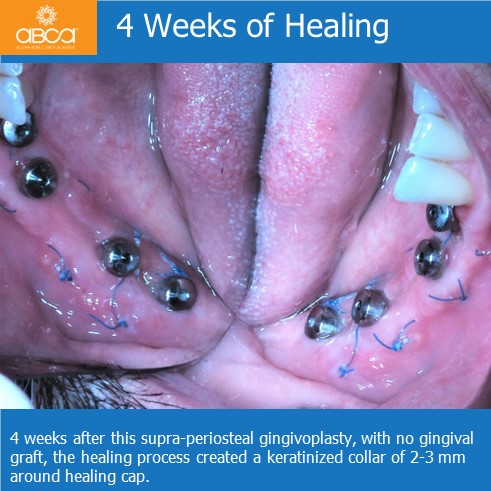
4 weeks after this supra-periosteal gingivoplasty, with no gingival graft, the healing process created a keratinized collar of 2-3 mm around healing cap.
Two years after surgery, there is stable attached gingiva and bone around implants.